Your Guide to the Gastro Bug NZ
We’ve all heard it, and most of us have unfortunately experienced it: the dreaded "gastro bug". In New Zealand, this is the common term we use for gastroenteritis, a nasty inflammation of your stomach and intestines.
It’s usually caused by a virus, with the two most common offenders being norovirus and rotavirus. These are highly contagious and are often the reason a tummy bug can rip through a household or a classroom so quickly.
Unpacking the NZ Gastro Bug
So, what’s actually happening when you catch a gastro bug?
Think of these viruses as tiny invaders that set up camp in your digestive system. Once they're in, their only goal is to multiply, which throws your body's normal processes into chaos and triggers a full-blown immune response.
This internal battle is what causes those all-too-familiar symptoms. Your body is essentially trying to evict the invaders as forcefully and quickly as it can, leading to vomiting and diarrhoea. It feels absolutely miserable, but it's your body’s natural defence system kicking into high gear.
The Main Viral Culprits in New Zealand
Not all gastro bugs are identical. Here in New Zealand, a few specific viruses are behind most of the misery. Knowing a bit about them helps clarify why these bugs spread like wildfire.
-
Norovirus: This one is famously known as the "winter vomiting bug." It's incredibly infectious and can survive on surfaces for days. You only need to come into contact with a tiny amount of the virus to get sick, which is why it’s notorious for outbreaks in schools, rest homes, and offices.
-
Rotavirus: This virus is the leading cause of severe diarrhoea in babies and young children. The good news is that the rotavirus vaccine is part of the standard childhood immunisation schedule in NZ, which has dramatically cut down on severe cases among our tamariki.
-
Adenovirus: While we often associate this one with colds and respiratory issues, some strains can also cause a nasty bout of gastroenteritis, particularly in kids.
The key thing to remember is that the "gastro bug" isn't a single entity. It's a catch-all term for a set of symptoms caused by several different, and very effective, viruses. Their knack for spreading easily is what makes gastro such a common headache for whānau across the country.
How Does the Gastro Bug Spread So Easily?
The way gastro bugs are transmitted is remarkably simple and efficient, which explains why they can take down an entire family in a matter of days. The main pathway is what’s known as the faecal-oral route. It sounds gross, but it just means the virus travels from the poo or vomit of a sick person to the mouth of someone else.
This typically happens in a few ways:
-
Direct Contact: Looking after someone who is sick or even just shaking their hand can be enough to transfer the virus.
-
Contaminated Surfaces: The virus can linger on things like doorknobs, toys, remote controls, and benchtops long after an infected person has touched them.
-
Contaminated Food or Water: If someone who is sick prepares food, they can easily pass the virus on to everyone who eats it.
Because these viruses are invisible to the naked eye, strict hygiene is your best defence. Something as simple as washing your hands thoroughly and often can be the most powerful tool you have to stop an outbreak before it starts.
How Widespread Is Gastro in New Zealand?
Just about every Kiwi has a story about a miserable run-in with a gastro bug, but it’s easy to underestimate just how massive its impact really is. This isn’t just a few days of feeling rough; gastroenteritis is a major public health issue in New Zealand, causing serious disruption for families, schools, and workplaces right across the country.
When you look at the numbers, you start to see the true scale of the problem.
A landmark community study on acute gastrointestinal illness dug into the data and came back with some eye-opening figures. It found that in any given four-week period, a whopping 8.6% of New Zealanders will get hit with at least one bout of diarrhoea or vomiting. That works out to an average of 1.11 episodes per person, per year.
Think about that for a moment. When you apply that rate to the whole population, the numbers are staggering. We're talking about roughly 4.66 million episodes of gastro bug tearing through the country every single year. This shows it’s far from a rare inconvenience—it's a routine, and costly, part of life for millions. The study revealed this leads to nearly one million GP visits, over 300,000 courses of antibiotics, and more than 4.5 million days of paid work lost annually. If you're interested in the nitty-gritty, you can explore the full findings from the community study.
Who Is Most at Risk?
While anyone can fall victim to a nasty gastro bug, it definitely doesn't play fair. Some groups are far more likely to catch it and tend to suffer more severe symptoms. Knowing who is most vulnerable is the first step in protecting them.
Unsurprisingly, young children—especially those under five—are hit the hardest. Their immune systems are still getting up to speed and aren't quite ready to fend off aggressive viruses like norovirus and rotavirus. On top of that, places like daycare centres and kindies are perfect hotbeds for these bugs to spread like wildfire, thanks to close contact and a lot of shared toys.
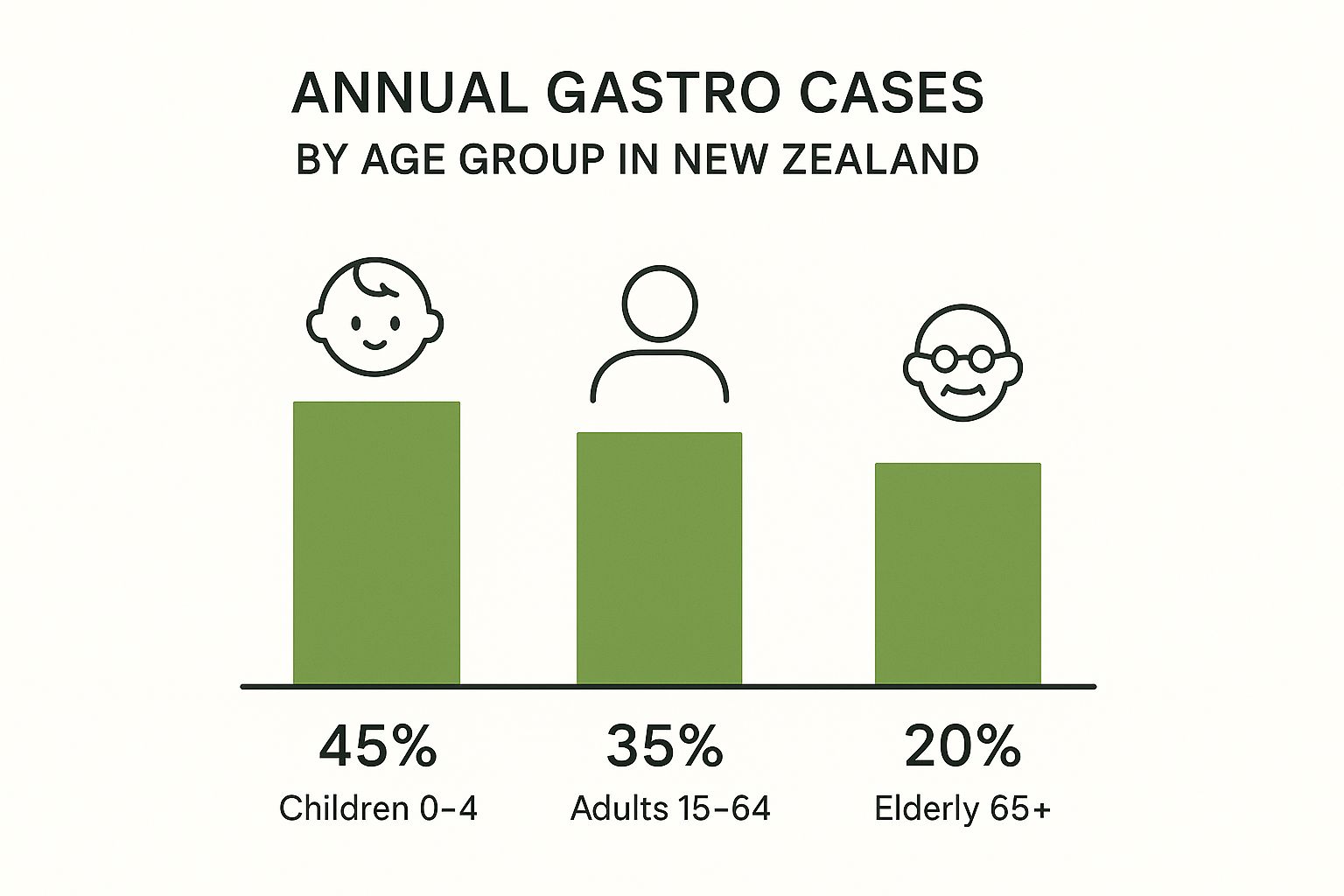
Our little ones account for the biggest slice of the pie, highlighting just how susceptible they are to the common gastro bug in NZ.
Vulnerability in Older Adults and the Immunocompromised
At the other end of the age spectrum, older adults aged 65 and over also face a higher risk, but for different reasons.
-
Weaker Immune Systems: As we get older, our immune response naturally slows down, making it tougher to fight off infections that we might have shaken off easily in our younger years.
-
Underlying Health Conditions: Many older Kiwis are already managing other health issues, like heart or kidney problems. The dehydration and physical toll from a gastro bug can seriously complicate these conditions.
-
Living Arrangements: People in rest homes or residential care facilities live in close quarters. Much like a daycare, all it takes is one person to get sick for an outbreak to sweep through the facility.
It's not just about age, though. Anyone with a compromised immune system is in a high-risk category. This includes people undergoing chemotherapy, living with an autoimmune disease, or who have had an organ transplant. For these individuals, what might be a standard gastro bug for someone else can quickly become a serious medical event that requires a hospital stay.
Recognising the Symptoms of a Gastro Bug
When a gastro bug hits, it rarely does so quietly. One minute you feel fine, and the next, you're hit with a sudden, intense wave of feeling unwell. It's an unmistakable sign that something is not right in your digestive system.
That initial queasiness is your body's alarm bell, signalling it's found an intruder. This feeling can escalate quickly, so it's a good idea to get comfortable and prepare for what's likely coming next.
The Unmistakable Signs of Gastro
The main symptoms of a viral gastro bug are pretty full-on, but they’re actually your body's way of fighting back. It’s trying to forcibly evict the virus, and while it feels awful, this aggressive response is a crucial part of getting better.
Here’s what you can typically expect:
-
Sudden vomiting, which can be quite forceful and frequent.
-
Watery diarrhoea, often starting a little while after the vomiting begins.
-
Stomach cramps and pain that can range from a dull ache to quite severe.
-
A low-grade fever, along with general aches, chills, and a feeling of complete exhaustion.
These symptoms usually kick in 12 to 48 hours after you’ve been exposed to the virus. Most people are through the worst of it within one to three days, with the first 24 hours often being the most intense.
Think of it like your body declaring war on the virus. The vomiting and diarrhoea are its most effective weapons, designed to flush the enemy out as fast as possible. This is why it’s so vital to support your body's efforts with plenty of fluids – you’re providing the backup it needs to win the fight.
Gastro Bug vs Food Poisoning
It’s incredibly easy to mix up a viral gastro bug with bacterial food poisoning. They look and feel very similar, but a few subtle clues can help tell them apart, especially how fast the symptoms appear.
Here's a handy guide to help you spot the difference.
Gastro Bug Symptoms vs Food Poisoning
|
Symptom / Feature |
Viral Gastro Bug (e.g., Norovirus) |
Bacterial Food Poisoning (e.g., Salmonella) |
|---|---|---|
|
Onset Time |
Typically 12 to 48 hours after exposure. |
Often much faster, from 1 to 6 hours after eating. |
|
Primary Symptoms |
Vomiting is often the first and most prominent symptom. |
Severe stomach cramps and diarrhoea are usually dominant. |
|
Fever |
A low-grade fever is common. |
A high fever is more likely. |
|
Source |
Spread from person to person or contaminated surfaces. |
Caused by eating food contaminated with bacteria or toxins. |
The main takeaway here is timing. Bacterial food poisoning from things like Salmonella or Campylobacter often hits much faster because you're reacting to toxins that were already in the contaminated food. A viral bug like norovirus, on the other hand, needs a bit of time to multiply inside your body before it triggers symptoms.
While it's useful to know the difference, the immediate at-home treatment for both is essentially the same: rest up and stay hydrated.
How to Manage Gastro at Home

When a nasty gastro bug hits, your home instantly becomes the recovery ward. It feels absolutely miserable, but the good news is that most cases can be handled safely without a trip to the doctor. The game plan is simple but non-negotiable: rest, rehydrate, and gently reintroduce food only when your body is ready.
You will likely be losing fluids from both ends and your body is getting dangerously parched. Your number one priority, above all else, is replacing the fluids and electrolytes your body is losing. Dehydration is the biggest risk with any gastro bug in NZ, so keeping on top of fluid intake is absolutely critical.
The Golden Rules of Hydration
Staying hydrated isn't just about chugging water; it’s about replacing the lost salts and minerals, too. The trick is to take small, frequent sips all day long. Gulping down a huge glass of anything is a surefire way to trigger more nausea or vomiting.
Here are your best bets for rehydration:
-
Oral Rehydration Solutions: You can grab these from any chemist. They’re the gold standard because they’re specifically formulated to replace water, salts, and sugars in the perfect balance your body needs.
-
Diluted Juice: If you can't get a rehydration solution, mixing one part fruit juice with four parts water is a decent backup. Stick to apple or grape juice and give citrus a wide berth.
-
Weak, Unsweetened Tea: Gentle herbal teas like peppermint or ginger can be incredibly soothing for a queasy stomach.
Just as important is knowing what not to drink. Sugary drinks like fizzy drinks, undiluted juice, and energy drinks are a terrible idea. They can actually make diarrhoea worse by pulling more water into your gut. Caffeinated drinks and milk should also be off the menu until you’re well on the mend.
Key Takeaway: The goal isn't just to drink, but to rehydrate effectively. Small, consistent sips of the right fluids are far better than large amounts of the wrong ones. This gentle approach gives your body the best chance to absorb what it needs without overwhelming your sensitive system.
Reintroducing Food Gently
Once the vomiting has stopped for a few hours and you start to feel the first pangs of hunger, you can think about food again. The key here is to start with incredibly simple, bland foods that won’t challenge your stomach. Don’t rush this step—listen to your body. If your symptoms flare up, back off.
A great place to start is the classic BRAT diet:
-
Bananas
-
Rice (plain and white)
-
Applesauce
-
Toast (dry, no butter)
Other safe options include plain crackers, boiled potatoes, or a clear, simple broth. You’ll want to avoid anything fatty, spicy, or heavy for a few days, as these can easily irritate your digestive system and set your recovery back. As you start feeling better, you can slowly work your way back to your normal diet. For anyone wanting to give their system some extra support long-term after an illness, reading up on gut health supplements can offer some really useful ideas for restoring that crucial balance.
Special Care for Children and the Elderly
When a gastro bug strikes young children or older adults, you need to be extra vigilant. They can become dehydrated much, much faster. For babies, keep offering breast milk or formula, just in smaller, more frequent feeds. If you see any signs of dehydration, talk to your doctor or pharmacist immediately about a suitable oral rehydration solution.
With older adults, especially those with other health conditions, it's vital to monitor their fluid intake like a hawk and watch for signs of confusion or dizziness. Make sure fluids are always within easy reach and gently encourage them to sip regularly throughout the day.
Ultimately, managing gastro at home is all about supporting your body’s natural ability to heal. With plenty of rest, careful hydration, and a gentle return to food, you can help your family get through the worst of it and safely back on their feet.
How to Stop the Spread of Gastro
Once a gastro bug gets into your home, it can feel like a game of dominoes—you’re just waiting for the next person to topple. But you're not helpless. By taking swift and thorough action, you can absolutely contain the outbreak and protect the rest of your family.
Think of a gastro virus like glitter. The moment it's out of the container, it gets everywhere and is a real mission to clean up. Your best defence is to be meticulous with hygiene and disinfection, focusing on breaking that chain of transmission before it really takes hold.
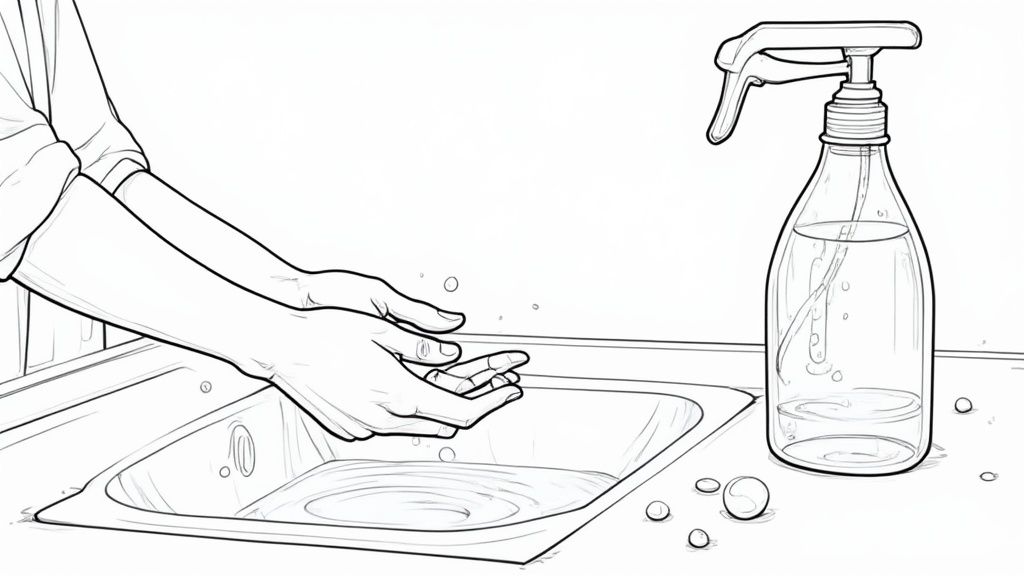
Master the Art of Handwashing
Hands down, the single most powerful tool you have against a gastro bug is proper handwashing. It sounds so simple, but it’s an area where many of us cut corners. When you’re up against something as tenacious as norovirus, a quick rinse under the tap just won’t do the job.
You need to get in there with soap and warm water, scrubbing for at least 20 seconds. A good trick is to sing "Happy Birthday" through twice in your head. It’s the physical friction from scrubbing that actually lifts the tiny virus particles off your skin so the water can wash them away.
Here’s the gold-standard technique:
-
Wet your hands with clean, running water.
-
Lather up with a decent amount of soap. Make sure you get the backs of your hands, between your fingers, and right under your nails.
-
Scrub with gusto for that full 20 seconds.
-
Rinse everything off completely under the running water.
-
Dry your hands thoroughly with a clean, dry towel or a paper towel.
It's also worth noting that alcohol-based hand sanitisers aren't nearly as effective against norovirus. While they’re certainly better than nothing in a pinch, they don't kill the virus as effectively as a good old-fashioned scrub with soap and water. Stick to the sink whenever you can, especially after using the loo or before touching food.
Create a Safe Zone for Food Preparation
The kitchen can easily become ground zero for spreading a gastro bug, making food hygiene non-negotiable during an outbreak. Many gastroenteritis outbreaks in New Zealand have been traced back to how food was prepared or handled. We've seen cases linked to everything from Clostridium perfringens in catered meals to Vibrio parahaemolyticus in raw mussels, which sickened dozens of people. It’s a stark reminder of how easily these bugs travel through what we eat.
If someone in your house is sick, the kitchen should be a no-go zone for them. Period.
And if you’re the one caring for them, you need to be extra vigilant:
-
Wash your hands meticulously before you start cooking and after you've finished.
-
Use different chopping boards for raw meats and fresh produce to avoid cross-contamination.
-
Make sure you cook food to the correct internal temperature to kill off any lurking germs.
Disinfect Surfaces the Right Way
Norovirus is a tough character. It can happily survive on surfaces like benchtops and doorknobs for days, and your usual all-purpose spray might not be enough to evict it. To really kill it, you need to bring out the big guns: a bleach-based solution.
For a powerful disinfectant, mix 1/4 cup of regular household bleach with 5 litres of water. Use this solution to wipe down all the high-touch surfaces around your home—think doorknobs, light switches, remote controls, taps, and benchtops.
When cleaning up after someone’s been sick (vomit or diarrhoea), always wear disposable gloves. Use paper towels to soak up the mess, seal them in a plastic bag before binning it, and then clean the area thoroughly with your bleach mix. Any contaminated clothes, towels, or bedding should go straight into the washing machine on the hottest cycle available. Alongside home hygiene, understanding effective strategies for preventing infections in public spaces can also help protect your family.
Finally, one of the most crucial steps is to keep the sick person at home. The golden rule is to stay away from work, school, or daycare for at least 48 hours after the last symptom has vanished. Even if you're feeling much better, you can still be highly contagious during this two-day window. While you're recovering, it's also a good time to think about long-term gut health; the connection between probiotics and immunity is a key part of building a resilient defence system.
When You Should See a Doctor
Most gastro bugs that do the rounds in NZ are miserable but short-lived ordeals you can ride out at home. Our bodies are pretty good at kicking these viruses to the curb, but sometimes, they need a bit of professional backup.
It’s a bit like a fire alarm in your house. A little bit of smoke from burnt toast is something you can sort out yourself. But when the big alarms go off, it signals a problem you need the experts for. Knowing the difference is key to a safe recovery.
If your symptoms start getting severe, like a raging fever or vomiting that just won't quit, it's time to think about professional help.
Key Warning Signs for Adults
For most healthy adults, the biggest risk from a gastro bug is severe dehydration. That said, there are a few other red flags that signal it's time to call your GP or head to an after-hours clinic.
Don't wait it out if you're experiencing any of these:
-
Signs of serious dehydration: This isn't just feeling thirsty. We're talking about not weeing for more than 8 hours, feeling dizzy or faint when you stand up, having a mouth that feels like sandpaper, or feeling confused.
-
Can't keep anything down: If you’re vomiting up every sip of water for more than 24 hours, you simply can't rehydrate yourself.
-
A high fever: A temperature that’s stubbornly sitting above 38.5°C and isn’t budging with medication is a clear warning sign.
-
Severe tummy pain: Cramps are part of the deal with gastro, but intense, sharp, or constant pain is not normal.
-
Blood in your vomit or stools: This is something that always needs to be checked out by a doctor, no exceptions.
These symptoms could point to a more serious infection or a level of dehydration that needs medical help, like fluids through an intravenous (IV) drip, to get you back on track.
When to Seek Help for Children and Babies
Kids, and especially babies, are a different story. Their little bodies can become dangerously dehydrated much, much faster than an adult's.
You must act quickly if you see signs of dehydration in a child. Trust your gut—if you are worried about your child, it is always best to get them checked by a doctor.
Get in touch with your doctor or local health service straight away if your baby or child has any of these signs:
-
For babies: Fewer than 4 wet nappies in 24 hours is a major red flag. Also, watch for no tears when they cry or a sunken fontanelle (the soft spot on the top of their head).
-
For any child: If they seem unusually drowsy, floppy, or are really hard to wake up.
-
Symptoms that drag on: If vomiting or diarrhoea lasts more than 12 hours in a baby or 24 hours in a toddler.
-
Refusing to drink: If they're flat-out refusing any fluids for several hours.
It's also worth noting that older adults and anyone with a weakened immune system should get medical advice sooner rather than later, as they're also at a higher risk of complications. When in doubt, making the call is always the safest option.
Frequently Asked Questions About Gastro in NZ
Even after you've weathered the worst of a gastro bug, it's normal to have a few questions hanging around. Let's tackle some of the most common things Kiwis ask when it comes to this nasty illness.
How Long Am I Contagious For?
This is the big one, and it's key to stopping the bug from spreading through your entire household or workplace. You're considered contagious from the moment symptoms start until at least 48 hours after your last bout of vomiting or diarrhoea.
It’s a tricky one because you might start feeling much better, but you can still be shedding the virus and passing it on. That two-day, post-symptom isolation period is non-negotiable if you want to protect your whānau and colleagues.
Can I Get the Same Gastro Bug Twice?
The short answer? Unfortunately, yes. Viruses like norovirus have many different strains circulating at any one time, so getting sick with one doesn't make you immune to the others.
On top of that, any immunity you do build up to a specific strain doesn't last forever. It fades over time, which means you could even get sick with the very same strain again a few years down the track.
This is exactly why you can't just rely on having "had it already". Good old-fashioned hygiene is always your best line of defence. Consistent handwashing and proper cleaning are your most reliable tools.
What Is the Best Way to Clean My House After a Gastro Outbreak?
When you're dealing with a tough virus like norovirus, your standard multi-purpose spray probably won't cut it. You need to bring out the big guns, and in this case, that means bleach.
-
Mix up your solution: Follow the instructions on a bottle of household bleach and be sure to dilute with water to create a proper disinfecting solution.
-
Wipe down everything: Go after all the high-touch surfaces – think doorknobs, light switches, taps, remote controls, phones, and kitchen benchtops.
-
Hot wash is best: Throw any contaminated bedding, towels, and clothing into the washing machine on the hottest cycle the fabric can handle.
Once the house is clean and you're on the mend, your focus can shift to helping your gut recover. A good dose of probiotics can make a real difference. You can learn more about how to use natural probiotics to help your digestive system bounce back.
Ready to support your family's gut health and build a stronger defence against common bugs? Explore the Rawbiotics range of natural, live liquid probiotics. Find the perfect blend for your whānau at https://www.rawbiotics.co.nz.