Probiotics After Antibiotics A Practical Gut Restore Guide
Taking a course of antibiotics is often a necessary part of getting well, but these powerful drugs can be pretty rough on your gut. Once you've finished the course, you might feel like you've won the battle, but the cleanup has just begun. Thinking about probiotics after antibiotics isn't just following a health trend; it's a smart, practical step to help your body recover properly and get you back on your feet faster.
Why Your Gut Needs Some Help After Antibiotics
Imagine your gut is a lush, thriving garden. Antibiotics are a bit like a powerful, non-selective weedkiller. They do a fantastic job of wiping out the nasty bacteria making you sick, but they can't distinguish between those "weeds" and the beneficial "flowers" that keep your gut garden healthy and in balance.
This collateral damage creates what's known as microbial dysbiosis—a fancy term for a gut flora that’s been thrown completely out of whack.
This isn't a small problem. The disruption often leads to some pretty immediate and uncomfortable digestive complaints, such as:
-
That awful bloated feeling and excess gas
-
Antibiotic-associated diarrhoea (AAD)
-
General irregularity and stomach upset
For a lot of people, these aren't just a fleeting issue. A compromised gut microbiome can take weeks, sometimes even months, to sort itself out on its own. This can leave you feeling subpar and even vulnerable to other problems long after the original infection has cleared.
The Bigger Picture in New Zealand
The conversation around gut support is more relevant than ever, especially here at home. Data shows that between 2006 and 2014, total antibiotic use in New Zealand shot up by a staggering 50%. A huge part of this jump was driven by a near-doubling in the prescription of common penicillins like amoxicillin. You can dive deeper into the numbers by checking out the full report on these antibiotic consumption trends.
What this really highlights is that more and more Kiwis are dealing with the fallout from these essential medicines. It’s a classic scenario: someone takes amoxicillin for a nasty chest infection, gets better, but then spends the next month battling frustrating digestive issues. This happens all the time, and it’s precisely why being proactive about rebuilding your gut flora is so crucial.
Once you grasp that antibiotics cause this kind of widespread disruption, it’s easy to see why just sitting back and waiting for your body to fix itself isn't the best plan. Actively giving your gut the support it needs helps bring back balance, eases those uncomfortable side effects, and lays the groundwork for better digestive health in the long run. It's really about giving your body the right tools to rebuild its internal ecosystem.
Getting the Timing Right with Your Probiotics
One of the first things people ask is, "When exactly should I start taking probiotics?" It’s a smart question, because with this, timing is everything. If you take them too close to your antibiotic dose, you risk the medication wiping out the very bacteria you’re trying to introduce. But if you wait until the course is over, you might be stuck with an upset gut for longer than necessary.
The trick is to get those good microbes back into your system without putting them directly in the line of fire. It's like trying to plant a new lawn; you wouldn't scatter seeds while the weed killer is still fresh on the soil. You need to give it a little time to settle so the new grass has a chance to take root.
The 2-to-3-Hour Rule
So, how do you do it? The best approach is to take your probiotics during your antibiotic course, but you need to be strategic about it. A good rule of thumb is to leave a gap of at least 2 to 3 hours between your antibiotic and your probiotics.
This simple buffer creates a window of opportunity for the good bacteria to arrive and start colonising your gut without being immediately wiped out.
For instance, if you take your antibiotic with breakfast at 8 am, plan to take your probiotics with lunch. If your second antibiotic dose is at 8 pm, you could take your probiotics mid-afternoon or a few hours before bed. This spacing is probably the single most effective thing you can do to make your probiotics work while on antibiotics.
Expert Tip: Don't stress about hitting the 2-hour mark perfectly. The goal is simply to create a clear separation. This small habit gives your probiotics the best chance to do its job, even while the antibiotics are still active.
Don’t Stop When the Antibiotics Do
Your gut recovery mission doesn't finish when you swallow that last antibiotic pill. Even though the medication is out of your system, your gut microbiome is still in a vulnerable state, like a cleared-out field waiting to be replanted.
Continuing with probiotics after antibiotics is vital for a full recovery. It provides a constant stream of beneficial bacteria to fill up the 'empty space' in your gut, helping to bring back balance and strength.
How Long Should You Keep Going?
-
At a minimum: Keep taking your probiotic for 2 to 4 weeks after your last antibiotic dose. This gives your gut a solid head start.
-
For a full recovery: If you’ve been on a particularly strong or long course of antibiotics, I’d recommend continuing for 1 to 3 months.
This extended support gives your gut the time it needs to rebuild a robust, diverse community of microbes. Think of it as an investment in getting back to normal faster and building up your digestive resilience for the future.
However, many individuals discover that incorporating a probiotics into their daily regimen can assist in maintaining gut health, particularly because the levels of beneficial bacteria in our soils have decreased in recent times.
Choosing the Right Probiotic Strains for Your Recovery
Walking into a health store and staring at a wall of probiotics can feel pretty overwhelming. Dozens of bottles, all promising amazing gut health benefits. But here’s the thing: when you’re recovering from a course of antibiotics, not just any old probiotics variant will cut it. You need the right tools for the job.
Think of your gut post-antibiotics as a garden that's just been weeded a little too enthusiastically—it’s taken out the bad guys, but a lot of the good stuff has gone too. You wouldn't just scatter a random mix of seeds and hope for the best. You'd carefully select plants known to restore balance and thrive. The same goes for your gut microbiome.
This image really highlights the difference the right probiotics can make in how quickly you bounce back.
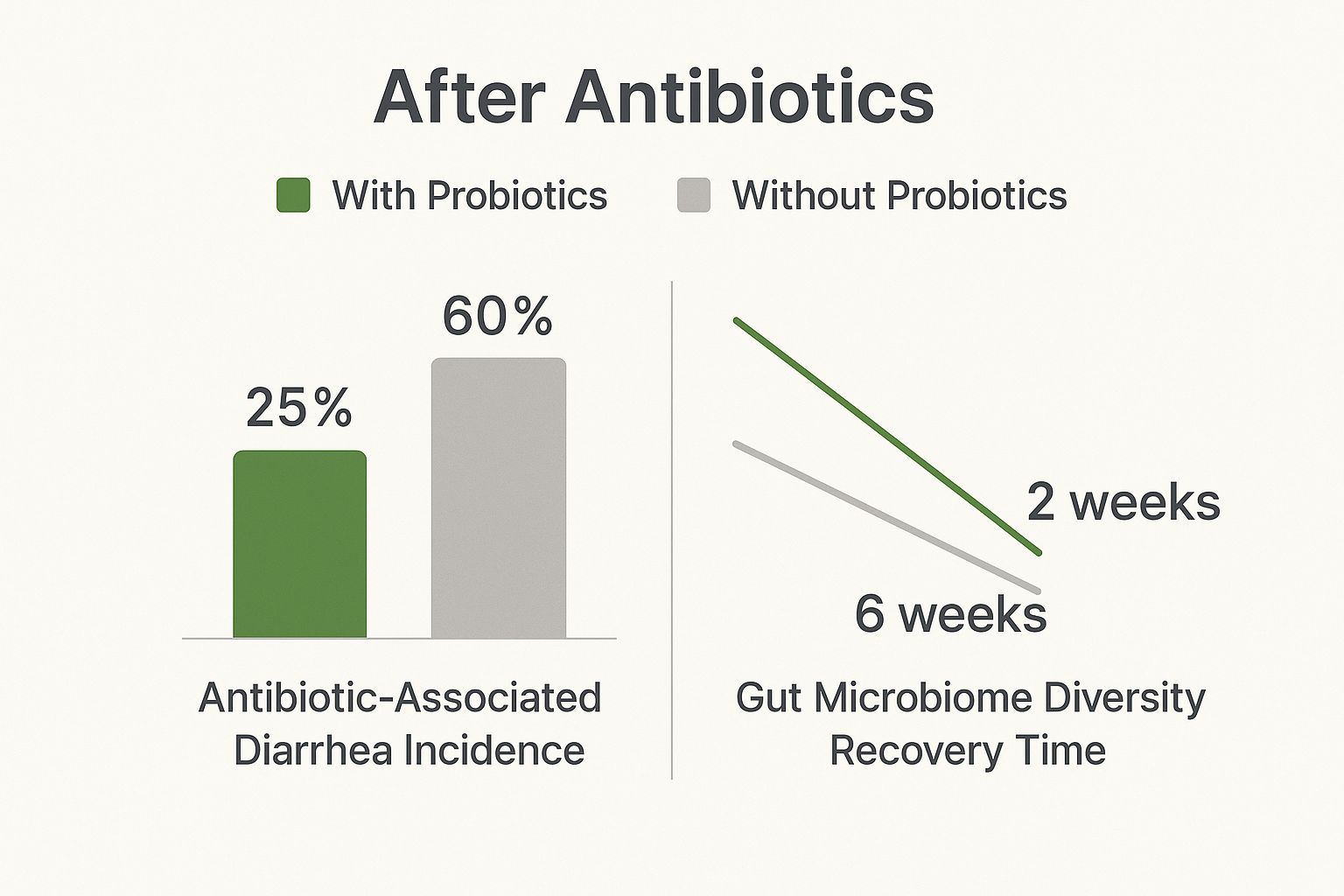
As you can see, targeted probiotics don't just speed up recovery; they can significantly reduce the chances of uncomfortable side effects like antibiotic-associated diarrhoea.
The Heavy Hitters: Key Strains to Look For
A broad variety of gut bacteria is important, but certain strains are especially beneficial for recovery after antibiotics. Here are the strains to look for when checking labels:
-
Bacillus subtilis: Known for its ability to form protective spores, this strain can help maintain gut health by supporting beneficial bacteria and enhancing the gut barrier.
-
Bifidobacterium bifidum: This strain supports digestive health and enhances immune response, making it a useful ally in restoring gut balance after antibiotic use.
Spotting strains like these in a probiotics formula indicates a product geared towards supporting gut health during and after antibiotic treatment. For more information on the roles of different bacteria, explore our complete guide to probiotics for gut health.
Here's a summary of some strains that can assist in your recovery:
Key Probiotics Strains for Post-Antibiotic Care
|
Probiotics Strain |
Primary Benefit After Antibiotics |
Commonly Found In |
|---|---|---|
|
Lactobacillus acidophilus |
Helps control harmful bacteria, aids digestion. |
Yoghurt, kefir, miso, tempeh. |
|
Bifidobacterium longum |
Supports digestive health and helps in nutrient absorption. |
Fermented foods, probiotics supplements. |
|
Lactobacillus plantarum |
Aids in maintaining intestinal permeability and modulating immune function. |
Sauerkraut, kimchi, probiotic supplements. |
|
Streptococcus thermophilus |
Assists in lactose digestion and boosts gut flora. |
Yoghurt, cheese, probiotic supplements. |
Opting for a supplement featuring these strains can effectively aid in rebuilding a healthy and robust gut environment.
Understanding CFUs and Strain Diversity
Now, let's talk numbers. On probiotics labels, you’ll see the term CFU, which stands for Colony-Forming Units. This is simply the measure of how many live, active microbes are packed into each dose.
After antibiotics have cleared out a large portion of your gut bacteria, you need a potent formula to make a meaningful difference. A sprinkle here and there won’t be enough.
A good starting point is a probiotic with at least 5 to 10 billion CFUs per serving. If you've been on a particularly strong course of antibiotics, you might want to look for something in the 20 to 50 billion CFU range for more intensive support. If using a live non-freeze-dried multi-strain probiotic you can opt for a lower CFU count as tend to maintain their viability and effectiveness better, allowing them to thrive and multiply more efficiently within the gut.
Finally, remember that a healthy gut thrives on diversity. While LGG and S. boulardii are strong contenders of post-antibiotic environment, a formula that also includes a variety of other Lactobacillus and Bifidobacterium strains offers more comprehensive support. Think of it as assembling a team where each player has a unique skill. Together, they work to rebuild your complex gut environment far more effectively than any single strain could alone.
How to Create a Gut-Friendly Environment
Taking a good probiotic is a brilliant move after a course of antibiotics, but that's really only half the story. To get the full benefit, you need to be a good host. Your goal isn’t just to send in new troops of good bacteria; it’s to create an environment where they actually want to stay, settle in, and thrive.
Think of it like planting a new garden. You wouldn't just scatter some seeds and walk away, right? You’d give them rich soil, water, and sunlight to help them flourish. It’s the exact same principle for your gut microbiome. This means actively supporting your new probiotic allies with the right diet.
Feed Your New Gut Allies with Prebiotics
This brings us to one of the most vital concepts in gut health: prebiotics.
If you think of probiotics as the beneficial ‘seeds’ for your gut, then prebiotics are the ‘fertiliser’. They’re specific types of fibre that we can’t digest, but our good gut bacteria absolutely feast on them.
When you eat prebiotic-rich foods, you’re directly feeding and strengthening the helpful microbes you’ve just introduced. This helps them multiply and set up a strong, healthy colony, which is a non-negotiable part of bouncing back after antibiotics.
Simply taking a probiotic without providing prebiotics is like sending workers to a job site without giving them any tools. Feeding them ensures they can actually get to work rebuilding and restoring balance in your gut. Pre-biotic rich foods are your go-to over prebiotic supplements.
Your Prebiotic Shopping List
Luckily, you don’t have to go on a treasure hunt for prebiotics. They’re found in plenty of everyday whole foods. Here are some of the best sources to add to your grocery list:
-
Garlic and Onions: These kitchen staples are powerhouse prebiotics.
-
Leeks and Asparagus: Delicious and fantastic fuel for your good microbes.
-
Bananas (especially when slightly green): A great source of resistant starch.
-
Oats: A simple bowl of porridge is a wonderful prebiotic boost to start your day.
-
Legumes: Think lentils, chickpeas, and beans.
Making small changes, like adding sautéed onion to your meals or having a side of asparagus with dinner, can make a huge difference over time.
What to Avoid to Keep Your Gut Happy
Just as important as adding the good stuff is knowing what to limit. Some foods can feed the less desirable bacteria and yeasts in your gut, which can really undermine your recovery efforts.
During this crucial rebuilding phase, it’s a good idea to be mindful of your intake of:
-
Excessive Sugar: Unfriendly microbes love sugar. Cutting back on sweets, sugary drinks, and refined carbs helps starve them out.
-
Highly Processed Foods: These are often stripped of the fibre your gut needs and can contain additives that disrupt your microbiome.
The best strategy? Focus on a diet loaded with diverse, whole foods—lots of colourful vegetables, fruits, and fibre. This is how you roll out the welcome mat for your new probiotic residents and give them the best possible chance to restore harmony.
For anyone wanting to dive deeper into optimising their gut health, our article on the best gut health supplements has even more practical tips.
How to Read the Signs of Gut Recovery
So, you've started your probiotics after a round of antibiotics. It’s only natural to wonder if they’re actually doing anything. The good news is, your body will tell you. You just need to know what signs to look for.
Learning to read your body’s signals isn't just reassuring; it helps you see that you're genuinely on the right path to recovery.
Right after antibiotics, it's common for your gut to feel a bit chaotic. You might be dealing with persistent bloating, uncomfortable gas, completely unpredictable bowel habits, or just a general feeling of being wiped out. These are all classic signs that your gut's delicate ecosystem has been thrown off balance.
The Shift to Positive Signs
As you stick with your probiotics routine, you’ll start to notice some gradual but really encouraging changes. This is your gut flora beginning to rebuild itself.
Here’s what to watch for:
-
Your Digestion Settles Down: One of the very first things you'll likely notice is a return to regularity. Bowel movements become more predictable and comfortable, and that feeling of constipation or sudden urgency starts to disappear.
-
Less Bloating and Gas: As the good bacteria start to flourish again, they get to work breaking down food properly. The result? A noticeable drop in that uncomfortable bloating and excess gas.
-
Your Energy Returns: A healthy gut is crucial for absorbing nutrients. Once your microbiome is back in business, your body can pull more energy from your food, which helps shake off that lingering post-illness fatigue.
It’s so important to remember that gut recovery is a journey, not a race. Some people feel a difference within a week, but for others, it might take a few weeks to really turn a corner. Be patient and give your body the time it needs.
A New Zealand Perspective
For many Kiwis, this whole process is a familiar one. Antibiotic use in our communities is quite high—in 2018, 47% of patients who saw their GP walked out with a prescription.
With so many prescriptions handed out, especially over winter, knowing how to support your gut afterwards is incredibly important.
This is why being proactive really matters. When you combine a good probiotic with other gut-friendly habits, you’re setting yourself up for a much faster and smoother recovery. If you’re curious about adding food-based support, our article on natural probiotics is a great place to start.
Paying close attention to these small shifts is empowering. It lets you track your progress and celebrate those little wins on the way back to feeling great.
Common Questions About Probiotics and Antibiotics

When you're trying to get your body back on track after a course of antibiotics, it's natural to have a few questions. You want to do what’s best for your gut, but figuring out the right steps can feel a bit overwhelming.
Let's walk through some of the most common queries we hear. Here are some clear, practical answers to help you feel confident about your gut health recovery.
Can I Get Enough Probiotics from Food Alone?
While I’m a huge advocate for fermented foods like kimchi, kefir, and good-quality yoghurt for everyday gut maintenance, they often can't deliver the high-potency dose needed right after antibiotics. Antibiotics are like a wildfire, causing a major drop in your beneficial bacteria across the board.
A quality probiotic supplement is different. It provides a therapeutic dose—measured in billions of Colony-Forming Units (CFUs)—that’s specifically designed to actively repopulate your gut in a way food just can't compete with.
Probiotic-rich foods are your gut’s daily maintenance crew, keeping things running smoothly. A high-quality probiotic supplement is the specialised first-response team you call in after a major incident like a round of antibiotics.
How Long Should I Take Probiotics After Finishing Antibiotics?
This is a really important question, because consistency is everything when you're rebuilding your microbiome. As a general rule of thumb, plan to keep taking your probiotic for at least 2 to 4 weeks after your last antibiotic pill.
But that's just the starting point. Research actually shows it can take several months for your gut microbiome to fully bounce back to its original diverse and resilient state. That’s why many health practitioners, myself included, often recommend a longer course of 1 to 3 months, particularly if you’ve been on a strong or prolonged round of antibiotics.
The best advice? Listen to your body. Keep taking the probiotics as long as you feel they’re helping your digestion and getting you back to feeling normal.
Are There Any Side Effects of Taking Probiotics?
For the vast majority of people, probiotics are incredibly safe and well-tolerated. When you first start, you might notice some mild, temporary side effects like a bit of extra gas or bloating.
Don't panic! This is usually just a sign that your gut is adjusting to all the new, friendly bacteria setting up shop. Think of it as a "settling in" period.
If you want to minimise any potential discomfort, try this simple trick:
-
Start with a half dose for the first few days.
-
Once your body feels adjusted, slowly work your way up to the full recommended dose.
If any symptoms feel severe or don't ease up after about a week, it's a good idea to stop and have a chat with your healthcare provider. Sometimes, a different probiotic strain or formula might be a better fit for your unique system.
Should Children Take Probiotics After Antibiotics?
Absolutely. Giving children probiotics after a course of antibiotics is highly beneficial. A child’s microbiome is still developing, which makes it particularly vulnerable to the disruptive force of these medicines. Here in New Zealand, antibiotic use is quite high among young kids, so this recovery step is even more critical.
The key is to use a product specifically formulated for a child's age and needs. Look for formulas containing well-researched paediatric strains like Lactobacillus rhamnosus GG or Bifidobacterium lactis, which have a great track record for its effectiveness in children.
As always, consult your GP or paediatrician before starting any new supplement. They can point you to the right product and dosage, ensuring your child gets the best possible support to help their gut recover, bounce back faster, and build long-term digestive and immune health.
Ready to give your gut the specialised support it needs to recover and thrive? The live, liquid cultures in Rawbiotics are designed to go to work immediately, helping restore balance with a synergistic blend of 12 powerful probiotic strains. Explore our range and find the perfect fit for your family's gut health journey at https://www.rawbiotics.co.nz.